
Like many industries, healthcare in Australia is in the midst of significant transformation. Rapid digitisation, increasing and changing demand for services, evolving community and government expectations and major investments in health infrastructure are driving well documented changes across the healthcare system.
The impact of these changes on the existing healthcare workforce is significant. The healthcare sector is the biggest growing sector in Australia in terms of workforce (at 14 per cent followed by education and training at 11.2 per cent).1
Workforce demand in the health sector, according to the federal government’s labour forecasts, will increase by 14.9 per cent over the next five years.2 However, it is also forecasted that the healthcare industry will experience major workforce shortages over the coming years due to an ageing healthcare workforce and current retention challenges, especially in regional areas.
Healthcare organisations need to manage the transition of current employees to potentially new and different ways of working. They also need to consider the requirements of a future workforce capable of delivering health outcomes in a healthcare landscape very different to that of today.
The healthcare workforce of the future will require its professionals to work increasingly in multi-disciplinary teams, while our healthcare systems will have to balance the benefits of technology and artificial intelligence (AI) alongside the ever present need for the ‘human touch’.

Workforce strategies and considerations
A number of workforce strategies are required in the coming years to manage these future challenges and opportunities. Three in particular are not only foundational but at this stage have the highest potential to benefit preparations for a ready and capable health workforce in the future.

Change of focus
All occupational groups will need to increase their focus on the management of patients outside the traditional healthcare setting, including remote monitoring, case management and preventative care.
Such a shift will require healthcare workers to consider, coordinate and review care differently. Importantly, this will require a behavioural transformation that supports an outcome-focused, collaborative and coordinated approach to patients and their health journeys. It will be a requirement of all healthcare workers, not the single domains of GPs and hospitals, to use the data and networks available to coordinate, collaborate and cooperate.
Collaborative education and partnerships
While this shift needs to occur within the healthcare setting, it also needs to translate into how new entrants to the workforce are prepared for their roles.
Curriculums delivered by educational providers will need to be co-designed with the health sector to ensure that the required capabilities and understanding of integrated models of care are prioritised, a focus that differs from the discrete traditional subjects or specialties typically taught in isolation. Such curriculums should focus on defining and introducing ‘on-the-job’ behaviours and mindsets that support collaboration and encourage health professionals to consider holistic responses to cases. Examples include cross-industry training that enables new entrants to understand system interdependencies, influences and opportunities. Such training is important in encouraging the future health workforce to innovate and solve complex problems in new ways.
Reinforcing these mindsets also requires new operating models based on strong ongoing partnerships between healthcare organisations, education providers and research institutions that push the boundaries of traditional healthcare - not just to leverage technology in healthcare, but to challenge and reshape the health ecosystem.
Collective leadership
A shift to collective leadership is also required. Collective leadership prioritises high-performing leadership teams over individuals and self-interest. Such a leadership style requires leaders who thrive in a changing environment, can make sound judgements about multiple competing perspectives and act mindfully with a deep sense of their own context and resilience.
Significant and ongoing culture change is at the heart of this new world. Leaders will need to collaborate with the workforce to identify elements of the culture that need to change and get feedback from people across all levels of the organisation. They will need to connect with a cross-section of the workforce who have insight into what people care about most. The focus then becomes adopting the few critical behaviours identified as mattering the most, demonstrating commitment by modelling these behaviours and committing to the change as a continual, collaborative effort.
The changes that are required should not be underestimated. Some employees will be energised, but some may resist.

Life-long training aligned to need
The effective use of new technology will be crucial to ensure optimal and efficient delivery of services and will require the health workforce to continuously learn, update and adapt skills to new operating environments.
Planning for the requisite health workforce skill set should be done with an awareness of the talent pipeline and the skills taught at schools and universities, and an eye to the future requirements posed by technological innovations. Programming, data analytics and human behaviour may need to be integrated into medical curriculums alongside anatomy and neurology.
The anticipated changes to workforce roles present an opportunity to redeploy, upskill or reskill employees. The sector will need to articulate and continue to evolve requisite skills and capabilities, using recruitment and retention strategies anchored to future needs.
Planning for the impact of technology, and therefore the required workforce, on health service delivery needs to be done now. The organisational arms for training and development need to work closely with those for technology and operations to assess new skill requirements and to ensure sufficient time is built in to train the workforce appropriately. Failure to strategically consider and develop the critical skills required for the future will adversely compromise the capacity of healthcare organisations to deliver services safely.
Retaining the human touch alongside AI
The introduction of technology such as robotics, AI and genomics will challenge the traditional roles of the healthcare workforce, including doctors.4 Digital and technological solutions will automate some work, dispense with some traditional roles and augment human effort.
For example major disease areas that currently use AI diagnostic tools include cancer, neurology and cardiology. AI helps to unlock the vast amounts of available but unstructured health data to enable more accurate diagnoses at an exponentially faster rate than a human being. As such the greatest impact of technological innovations on jobs in healthcare in the immediate future will likely be in medical diagnosis. 5
However, as technical tasks become automated and the human workforce work more and more alongside virtual assistants, the ‘human’ and personal aspects of care will become ever more important. This shift requires that the workforce will need to operate at the top levels of their
qualification and use their skills in an optimal way. AI and robotics technology will free up clinicians for other types of work that enable them to spend more meaningful time with their patients.
Leaders will need to be much clearer about their reskilling strategy and what that really means for their workforce. Which soft skills are required alongside digital skills? The nurturing of human qualities in the workforce, particularly leadership, creativity, empathy and curiosity, are essential to making the most of new technologies. Although functional skills related to automation and AI are often essential, they will not work without more ‘high-touch’ managerial and people-oriented capabilities.

New talent pipelines
The healthcare sector needs to develop proactive and creative solutions to attract, develop and retain the skills, capabilities and talent needed to deliver services, with a strong focus on diversity and inclusion, reflecting the community and its needs. Consideration of multiple talent pipelines will be critical, including leveraging immigration options to increase the supply of identified critical skills. Importantly, immigration and corresponding workforce policies will need to be coherent with international sourcing strategies to supply key talent, and industrial barriers and challenges will need to be worked through strategically.
Optimising current employment models and promoting greater cross-sector and cross-government collaboration to attract and retain critical skills may be key to addressing supply concerns.
A critical aspect will be to develop a compelling employee value proposition tailored to key segments of the workforce (eg. the proposition for a nurse will be quite different to that of a physician) to attract, develop and retain talent, while delivering a unified and engaging purpose-driven vision for the future.
Flexibility and agility
Flexible resourcing may also offer opportunities to explore alternative models of practice and partnerships enabling a shift to more agile structures and ways of working and enabling healthcare organisations to have the right skills in the right place at the right time to meet demand. This will make it possible for organisations to find the right mix while maintaining focus on workforce affordability.
Importantly, this strategy will need to be underpinned by contemporary workforce policies and practices that support the shift in model of care delivery including a consideration of how it will affect existing employment arrangements and operational practices within and across organisations.
Start from where you are
To prepare your healthcare workforce as you look to the future, you will need to consider all aspects such as culture, technology and ways of working. However, one critical step that healthcare organisations need to undertake now is strategic workforce planning to assess the sector's capabilities, supply challenges and shortages.
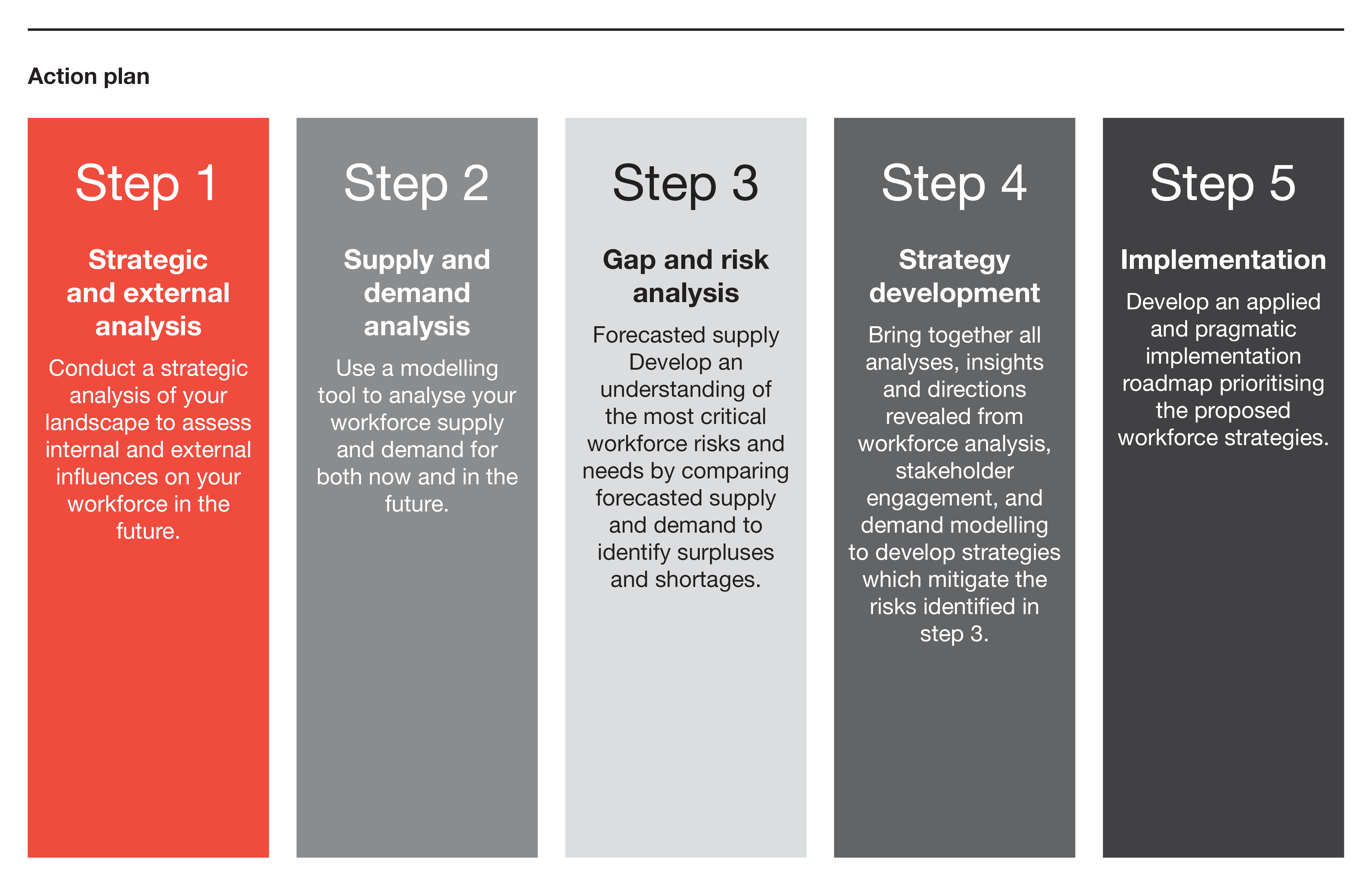
Strategic workforce planning enables organisations to evaluate the impact of global, national and local trends, and develop the essential initiatives to prepare their workforce for the future (eg. upskilling in new technologies or procedures; addressing potential resource gaps in critical roles or regional areas).
By understanding and setting future workforce requirements in the health sector, including the skills required to use and optimise technologies, a strategic workforce planning process can support and sustain a coordinated, collaborative and patient-centric approach to delivering care.
A strategic workforce planning approach can help healthcare organisations navigate through the complexity of their current and future operating environment to ensure a capable, appropriately sized and sustainable workforce. It aligns organisational and workforce strategies with macro trends, forecasts workforce supply and demand in line with service projections, and adopts an evidence-based approach to support targeted workforce interventions.
These steps should be supported by a series of stakeholder consultations to ensure an endorsed and pragmatic roadmap that when implemented will transform your workforce.
Rapid and diverse changes in the healthcare sector are in train, with more expected in the future. To ensure that it continues to be responsive to community needs, and the workforce continues to be capable of delivering positive patient and community outcomes, the sector needs to develop early and proactive strategies to transition to effect positive cultural change. Proactive planning and preparation today with an eye to tomorrow is critical; the health of the country’s future generations depend on it.
1 Australian Institute of Health and Welfare, Australia's health 2018, 2018
2 Australian Government Labour Market Information Portal, Health Care and Social Assistance, viewed July 2019
3 PwC Australia, Practical Innovation: Closing the social infrastructure gap in health and aging, February 2018
4 PwC Australia, Adopting AI in healthcare: why change?, February 2019
5 PwC Global, From Virtual to Reality: Six imperatives for becoming an AI-ready healthcare business, 2019















