
Our healthcare professionals do an amazing job considering the incredible demands placed on them. We require them to be caring, compassionate and resilient. And in addition to being expert problem solvers we expect them to support and comfort us when we are at our most vulnerable. They carry out their roles in an environment characterised by high complexity, high variation, high pressure and very low margin for error. But while we have one of the best hospital systems in the world in Australia, hospital errors continue to occur at unacceptable rates here and across the globe.
Healthcare is considered to be a 'safety-critical' industry. In this sense it can be compared to other industries such as aviation, nuclear power and even resources where risks are prevalent; and the consequences of errors can be catastrophic. These industries depend on their exemplary safety records to meet not just regulatory requirements but also the social licence to continue to operate. They achieve this by establishing internal structures, controls and procedures that reliably achieve optimal safety outcomes categorising them as high reliability organisations, or HROs.
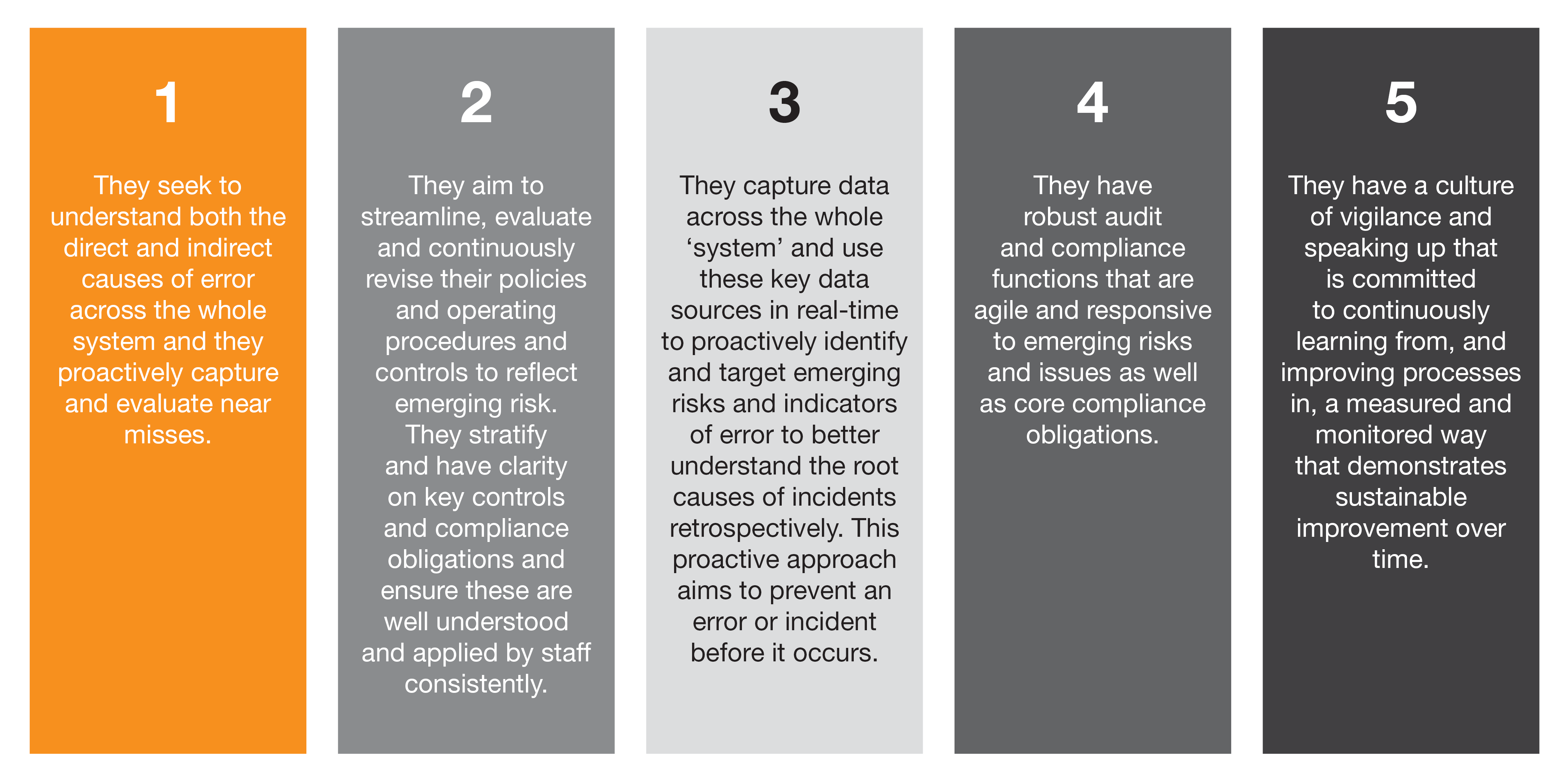
In essence, high reliability can be described as the means by which desirable outcomes are consistently achieved. Some of the key attributes of HROs include:
For over a decade, the healthcare industry has been conducting research into HROs and the lessons it can draw on. Despite a number of studies and pilots, progress in the healthcare setting appears to be limited. This is particularly evident when we consider the statistics.
- A recent study by Johns Hopkins reported more than 250,000 people in the United States die every year because of medical errors, making it the third leading cause of death after heart disease and cancer.1
- The World Health Organisation states there is a one in 10 chance of being harmed in hospital and 50% of these incidents and adverse events are preventable.2
- The Grattan Institute’s Safer Care Saves Money reports one in every nine patients who go into hospital in Australia suffers a complication – about 900,000 patients each year. If they stay in overnight, the figure rises to one in four – about 725,000 patients each year.
These hospital-acquired complications cost the Australian economy more than $4 billion a year.3

Source: Johns Hopkins
Why business as usual is not an option
The Australian healthcare system is recognised as one of the best in the OECD. However, as with any other advanced healthcare system, there are still a large number of preventable errors, complications and deaths every year. According to the 2018 Grattan Safer Care Saves Money report if the safety performance of all hospitals were lifted to the level achieved by the top 10 percent of hospitals, it would make a realistic reduction in complication rates to the value of AUD1.5 billion a year and would lead to an additional 250,000 patients leaving hospitals complication-free.
We believe that if we are to transform our health providers into HROs we need to be more strategic and challenge current thinking. To this end PwC has reviewed numerous cases and papers on safety in healthcare and other industries to try to identify any additional attributes and principles that define high reliability in a healthcare setting. Through this review, there were many examples where stark differences were evident in how the healthcare sector identifies and responds to incidents when compared with other industries.

One of the consistent themes we identified was the unnecessarily high level of process complexity, variation, ‘layering’ and duplication that was specific to the healthcare industry. The average health practitioner has far more 'mental work demand' placed on them than workers in other safety-critical industries. As humans we can only remember so many things and so there is a tipping point at which more results in less: less risk management, less compliance and less impact on patient safety.
In the workplaces we reviewed we found there were, on average, many thousands of compliance obligations, policies, procedures and forms.
Rather than examine the system as a whole more often than not the response to a new incident was to add further controls and compliance procedures, resulting in layering and ever-greater complexity. Frontline staff were continually bombarded with new interventions for short-term fixes and new activities they were expected to learn and implement. The end result was usually the opposite of what was intended; we found that too many activities made processes lengthy-layered and overly complex. This ultimately impacted the degree to which staff could remember and apply the most critical controls consistently and effectively.
When we looked at other safety-critical industries, it was clear that people working in HROs benefited from much more streamlined, simplified and effective systems of control. They are more equipped on the front line with an awareness of the key risks to safety in their roles and the key controls that they must perform each shift and each day to mitigate against this risk.
The concept of high reliability is not the result of a set of processes or an 'outcome'. As defined earlier it is the means by which desirable outcomes are consistently achieved.

Adopting a HRO model for healthcare
We used these insights to develop a high reliability framework that could be applied to healthcare. It incorporates the principles of system-based thinking, continuous improvement based on impartial feedback, the implementation of mature risk and compliance functions and effective use of data to evolve a culture of collective achievement across the entire organisation (see Figure 2).

1. System-wide thinking
System-wide thinking requires the organisation to understand which risks are a priority, including direct and indirect sources of error and to consider the full system of control when implementing significant process changes. Importantly, changes tend to be implemented at an industry level rather than a single organisation (think of pre-flight briefings in aviation).
2. Robust continuous improvement & feedback loop
HROs embed continuous learning into their feedback and audit tools to understand the root causes of error and risk. Feedback is actively encouraged and, rather than fostering a culture of blame, this information is used to understand and address potential risks or causes of error.
3. Mature risk compliance & audit functions
Organisations with a mature risk compliance and internal audit functions are both reactive and proactive, they are agile enough to be responsive to change and emerging risk while also aligning to strategy and providing comfort and insight on core compliance and control activities.
4. Effective monitoring & use of data
HROs collect data across the ‘system’, they use this data to proactively identify emerging risks and issues and to seek to address these before they occur. They collect data to assess compliance levels as well as to provide insight into emerging trends (eg. greater value placed on near-miss reporting and human factors such as engagement and behavioural risk trends) even using AI and pattern recognition software to anticipate risk and errors.
5. Culture of collective achievement
What evolves from this multi-faceted approach to high reliability is a culture of collective achievement where:
staff are engaged and understand clinical control activities and results;
new ideas and change are embraced to enhance compliance and reduce risk;
self-reporting is encouraged without fear of blame or sanction, and pro-safety behaviours are rewarded; and,
management take action on issues in a timely and visible manner so that staff see demonstrable measures are taken and change is made as a result of reporting.
The difference in approaches between HROs and healthcare is perhaps best demonstrated through a comparison of case studies from different industries. There is no shortage of examples to choose from, but here are two that clearly illustrate the point.

What action can you take right now?
It's complex and multifaceted but by going through this checklist you could identify some key areas that should be your priority focuses in your planning (checklist available in PDF for ease of use).
System-based thinking
1. When incidents and near misses occur do you consider the direct and indirect sources of error across the whole system? Do you consider what controls failed and why? Do you critically assess whether a new intervention should be implemented and whether activities and controls can also be removed?
2. Do you seek to reduce unwarranted variation in the system (e.g. streamline control activities and standardise processes, forms, checklists etc)?
3. Where emerging risks, incidents or near misses occur that result in changes to processes and controls do you apply this change consistently and effectively across the system (the organisation, the health service, the health system)?
Effective use of data
4. Are you using system-wide data in addition to clinical KPI results in a proactive way to identify risks including: clinical audit results; timely staff engagement and patient feedback results; HR data such as overtime, sick leave and agency usage etc?
5. Do you leverage data to identify recurring incidents and predict emerging risks and trends across the system and proactively review?
6. Do you leverage digital technology for audit and compliance activities to provide timely, accessible results to harness information and respond instantly?
Robust continuous improvement and feedback systems
7. Do you track, audit and monitor the new controls and interventions for effectiveness?
8. Do you capture your near misses and do you value and action this insight through sharing of lessons learned?
9. Do you have robust and effective continuous improvement plans as well as remediation action plans?
Mature risk and compliance functions
10. How confident is your Board that they have an integrated and complete assurance plan across the 'three lines of defence' (eg. clinical risk/audit and clinical internal audit)?
11. Do you have a robust and effective clinical governance framework with clearly defined accountabilities and responsibilities
12. Have you stratified and prioritised your key risks and controls by major clinical process areas and are your staff communicated to and trained on this? Do you seek to reduce variation, duplication and layering in processes and controls?
13. Does your clinical audit plan align to the major clinical process areas and reinforce staff awareness of key and critical control activities at the frontline?
14. Is your clinical audit plan agile enough to respond to emerging risks and strategic enough to get a balance between compliance, improvement and strategy?
15. Are you ‘everyday’ accreditation ready? Do you look beyond accreditation, seeing it as the minimum foundational requirement and not the end goal?
Culture and collective achievement
16. Do your staff feel comfortable speaking up for patient safety and are they respected and supported when they do?
17. Are your patients and consumers encouraged and educated on being active participants in the safety of their care and speaking up?
18. Is patient safety and quality paramount in your strategy and has this cascaded in a meaningful way from the board to the ward? Is it operationalised in such a way that all staff can articulate what this means for them, and how they bring it to life every day with their patients and residents and with each other?
19. Have you considered setting ambitious safety targets to track and report providing greater transparency? Do you hold each other to account and celebrate success together as a team?
20. Do you encourage and reward proactive and positive patient safety behaviours and do you share the stories within your organisation?
What can we do to target zero preventable harm in healthcare?
Hospital errors continue to happen and many are preventable. When we humanise the statistics and consider the devastating impact of preventable error on the families of the patients and on health practitioners, we are compelled to be relentless in our pursuit of zero preventable harm in healthcare.
We believe that the HRO approach exemplified by other high-risk, high-consequence industries such as aviation, nuclear power generation and resources can be applied to healthcare. However, due to the nuances of how healthcare is structured, its inherent risks, its delivery model and its culture, the focus areas we think the health sector should prioritise include addressing:
the complexity and unwarranted variations in processes
the lack of availability and use of timely system-wide data sources
Through implementing the high reliability framework healthcare providers can make a cultural change; one that rewards speaking up and avoids blame, monitors compliance while proactively anticipating possible risks and takes a system-wide view of risk management.
The benefits of greater reliability for patients are obvious: a better in-hospital experience, faster discharge and crucially, a reduction in the number of preventable illnesses, complications or deaths.
As consumers become increasingly better informed and discerning in their choice of care provider we see that organisations capable of implementing such an approach will be rewarded, not just through becoming an employer of choice for healthcare professionals, but also as a provider of choice for patients and their families.
1 Johns Hopkins Medicine, Study Suggests Medical Errors Now Third Leading Cause of Death in the U.S., 2016
2 World Health Organisation, 10 facts on patient safety, March 2018
3 Grattan Institute, All complications should count, 2018
4 Grattan Institute, Safer Care Saves Money, 2018















